Parkinson's disease (PD onwards) is an incurable neurodegenerative disease of the central nervous system, only relievable by drugs or neurosurgery, not preventable, progressive, with a tendency to invalidation. It is not fatal. It is produced by the degeneration of neurons that secrete a specific neurotransmitter, Dopamine, in the midbrain area known as the basal ganglia; specifically, up to 70% of the dopaminergic neurons of the "substantia nigra" and the striatum are lost. Dopamine is an important neurotransmitter necessary for the regulation of movement, gait and balance. In this PsychologyOnline article, we will talk about the Neuropsychology of Parkinson's Disease.
Index
- About Parkinson's disease.
- Mild and medium cognitive impairment.
- Dementias
- Other neuropsychological signs.
- Neuropsychological cognitive evaluation.
- Complementary tables
About Parkinson's disease.
PD is the second neurodegenerative disease after Alzheimer's disease. Some 110,000 people are affected in Spain. It affects males as well as females, and especially the most successful people (1.7% of those over 60 years of age), although 20% of the patients are under 50 years of age. Its causes are multiple and not yet fully known: genetic, metabolic, apoptosis, cellular oxidation, environmental toxins, ancient brain microtrauma, etc.
It is not a recent disease: it was already described magisterially in 1817 by Sir James Parkinson, who baptized it with the name of "Shaking Paralysis", thus highlighting its two components: akinesia (paralysis) and the earthquake (agitation). In fact, the four clinical criteria for its diagnosis are:
- Tremors of 4-8 Hz, predominance of rest.
- Bradykinesia, or generalized slow motion of movements
- Stiffness, or muscle hypertonia
- Balance disorders (falls, freezing of movements)
Although motor symptoms are the most prominent and main in PD, more and more attention is being paid to the existence of a parallel series of cognitive disorders and even dementia.
Mild and medium cognitive impairment.
A series of deficits of different basic mental functions (memory, attention, perception, mental agility, planning strategies, etc.), of different presentation by intensity and globality in each patient, but almost always present. Such deficit cognitive symptoms can be detected, in a very mild way, from the beginning of the diagnosis of the picture in patients not yet treated medically.
Although without showing a totally direct relationship, cognitive problems usually go in parallel with the progression and severity of the disease. When they appear very early, it is a poor prognostic index for the course of the disease, or it is not really known. It is a genuine PD but a related disease (diffuse Lewy body disease, cortico-basal atrophy, etc). We now go on to detail such typical cognitive deficits in PD, as they appear in the summary in TABLE 1.
BRADIPSIQUIA.
Most of the patients with PD show moderate to severe slowing down the speed of thinking and information processing, with increased neurological reaction time (P300 wave evoked potentials). For this reason, they take time to understand a question and generate an answer to a question, although the basic logic applied is not very altered.
MEMORY
Subjective complaints of "poor memory" are frequently reported by PD patients, but the complete amnesic syndrome typical of Alzheimer's does not appear. Long term memory It is more damaged than short-term memory, the other way around, for example, in Alzheimer's disease. The recognition of what has been learned (evocation with guides or aids) far exceeds what is remembered freely and spontaneously, what happens also in Supranuclear Palsy (PSP) but not in Alzheimer's (a disease that no longer benefits from "clues" to remember guided). Episodic memory (location of events in a spatio-temporal context) is somewhat burdened, also less than in Alzheimer's. Semantic memory (recall of general data), and the implicit (procedural, priming) are notably more preserved than in Alzheimer's. See TABLE 2. In general, PD shows slowness in memory and difficulties in accessing the stored data, which "is there", but the patient does not know well how to get there.
DIS-EXECUTIVE SYNDROME
The cognitive deficits of Problem resolution: planning and definition of objectives, sequencing of steps to achieve them, putting the plan into action, self-monitoring of the process (self-assessment), decision-making to modify the plans... The EP also shows poor mental flexibility and great cognitive rigidity, it is difficult for him to change strategies quickly, he tends to persevere in ideas (obsessive type pattern), it is not easy for him to handle two problems at the same time, scarce creativity... These symptoms are related to dysfunctions of the frontal lobes, and occur less intensely and later than in Huntington's disease or PSP.
ATTENTION
Show the EP deficit in maintaining active attention and concentration for a long time. He gets tired soon, and the emotional demotivation that the patient frequently shows collaborates. This also contributes to memory problems, because you do not remember well what you did not pay. attention (due to poor coding processes), and the decrease in the ability to learning.
PERCEPTIVE DISORDERS
Visuospatial perception is the one that is most centrally altered, apart from peripheral oculomotor problems. PD patients they do not perceive distances well, the relative position between various objects, the vision in three dimensions, the clarity of the images, it even seems that there is greater perseverance of the visual perceptions of what is due (visual sensory memory is not "erased" quickly, and earlier visual sensations may interfere with others new). In addition, the PD patient shows, like the PSP, difficulties in serving "multisensory" channels at the same time (eg, seeing and hearing simultaneously), powerfully interfering with these channels, mutually canceling or creating confusion.
Dementias
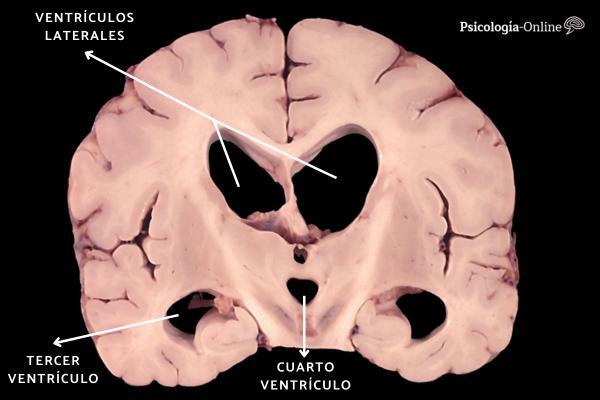
Didactically, two types of dementias can be differentiated: the cortical (Alzheimer's type) and the subcortical or frontosubcortical (Huntington type), whose characteristics I synthesize in TABLE 3. However, clinical practice shows many patients with mixed symptoms and transition pictures. Synthesizing, we would say that Alzheimer's Disease is the classic representative of cortical dementia, Diffuse Lewy Body Disease would show a mixed dementia both cortical As subcortical, PSP would be included in predominantly frontosubcortical and secondarily cortical dementias, and Parkinson's disease would be more representative of dementias subcortical. It is generally accepted that cortical dementias are more deteriorating than subcortical ones. We now detail the case of dementia in PD.
FRONTOSUBCORTICAL DEMENTIA
With the evolution of the disease over many years, almost one in three PD patients will show dysexecutive, bradyphrenic, and attention-memory problems so intense that interfere with their personal and social life in a clinically significant way, being able to give the diagnosis of "subcortical dementia" with a certain consistency conceptual. The problem is that the operational criteria for such a diagnosis are not clearly described in any manual international type DSM-IV of the APA or ICD-10 of the WHO, nor is there a standard neuropsychological battery with cut-off points precise. This type of dementia occurs with less incidence in genuine Parkinson's (idiopathic) than in Parkinsonisms such as multisystemic atrophies (Shy-Drager syndromes) or PSP.
CORTICAL DEMENTIA
Classic cortical symptoms such as deep amnesia, apraxia, aphasia, agnosia, and complete disorientation are rare in PD. The diagnosis of "Alzheimer's dementia" is not given beyond 10% of PD patients, although partial or partial cortical symptoms do appear. incomplete. It is important to point out that, given the advanced age of PD, this disease together with Alzheimer's can concur in the same patient at the same time, having to receive both diagnoses.

Other neuropsychological signs.
In the EP a series of emotional or character symptoms that can be related to the neurodegenerative disease itself (alteration of the balance between neurotransmitters: dopamine, acetylcholine, norepinephrine, serotonin, GABA; hypofunction of diencephalic and cortical structures) and not only as an experiential psychological reaction to suffering from a chronic disease, or as secondary effects of psychoactive medication.
Typical are references to depression (neurogenic-endogenous), apathy and apathy, flattening of the personality, emotional hyporeflexia, hyposexuality, obsession-compulsion, sleep disorders. Psychotic symptoms (hallucinations, delusions) and confusion do not belong to the natural history of PD, but are really unwanted side effects (iatrogenesis) induced by dopaminergic medication taken at high doses or during many years.
Neuropsychological cognitive evaluation.
Without wanting to be exhaustive, we will cite as useful in the EP: As extensive multidimensional batteries, the Barcelona de Peña-Casanova (PIEN-B) and version abbreviated (TB-A), the Wechsler WAIS-R scales, the Luria Neuropsychological Examination, and the Cambridge Cognitive Examination (CAMCOG, which is part of the most broad CAMDEX). Rapid tests to assess cortical deficit or dementia can be the Mini Mental (Flostein's MMSE and Lobo's MEC Spanish version) and the Shulman Clock Test (CDT). Also scales such as the Blessed Dementia Assessment (DRS), Hughes Clinical Dementia Assessment (CDR), Reisberg's Global Impairment Scale (GDS, FAS), and Informant's Test (TIN, Spanish version of the IQCODE of Jorm-Korten).
Specific tests are:
- The Front Function Evaluation Battery (FAB, studied in Spain by us) for the detection of frontal dys-executive syndrome;
- The Wisconsin Cards (WCST) for abstract reasoning and cognitive flexibility; the Color-Word Stroop for Response Interferences;
- The TAVEC as proof of verbal memories; the Rivermead (RBMT) as a procedural-behavioral memory test; the Memory Failure Questionnaire (MFE) for subjective complaints;
- The Bender-Rey-Benton (TGVM-TFC-TRVB) in visual-spatial, execution and visual memory skills; the Tracing Test (TMT AyB, Halstead-Reitan) as a visual-motor and conceptual test;
- Raven's Matrices as a test of the current level of abstract reasoning and the Word Accentuation Test (TAP) as an estimate of initial pre-morbid intelligence;
- The Tower of Hanoi and Kohs cubes in planning and problem solving. The evaluation is usually complemented with the Cummnings Neuropsychiatric Inventory (NPI) and the Yesevage Geriatric Depression Scale (GDS).
Complementary tables.
TABLE 1
NEUROPSYCHOLOGICAL DISORDERS IN PARKINSON'S DISEASE
1- Partial Cognitive Deficits
- Bradipsychia (slowness of thinking)
- Memory disorders
- Dis-Executive Syndrome
- Perception alteration (visuo-spatial)
- Low attention
- Little cognitive flexibility
- Mental fatigue
2- Dementias
- Frontosubcortical
- Cortical
- Mixed
3- Other disorders
- Flattening of the personality
- Apathy and abulia
- Anergy and areflexia
- Neurogenic depression
- Obsession-compulsion
TABLE 2
MEMORY ASSESSMENT
1- Subjective complaints from the patient
2- Sensory memories (immediate)
3- Short-term memory
- attentional component
- visuospatial component
- articulatory component
4- Long-term memory
- Declarative or explicit
- Semantics
- Episodic
- Procedural or implicit
- Priming
- Other behavioral
TABLE 3
TYPICAL CHARACTERISTICS OF DEMENCIES
Dementia: Cortical - Subcortical
Disease Alzheimer -Parkinson
Deterioration More homogeneous - Not Provided
Worse night Otherwise
Memory Olvidos, Amnesia - Difficult access
Orientation Disorientation-Oriented
Knowledge Agnosia - Bradipsychia
Execution Apraxia - Dissection
Language Aphasia - Normal
Speaks Initial normal - Dysarthria
Calculation Errors - Slowed
Cognitions Deteriorated - Poor use
Psychotic symptoms By illness - By medication
Affected Normal-Anxious - Depressive
Personality Normal-Inappropriate - Apathetic
Position Normal - Inclined
March Normal - Altered
Movements Normal - Slow
CoordinationInitial normal - Early affected
Cortex Affected - Variable affectation
Basal ganglia Little affected - Affected
Neurotransmitter Acetylcholine - Dopamine, others
Medium term fatal Otherwise
Quick test MMSE - FAB
TABLE 4
NEUROPSYCHOLOGICAL EVALUATION
1- level of general awareness
2- Temporal, spatial, and personal orientation
3- Attention and Concentration
4- Immediate, short-term, and long-term memory
5- Expressive and receptive language
6- Reasoning and Judgment
7- Gnosias (acknowledgments)
8- Praxias (skills)
9- Executive frontal capacities
10- Learnings
11- Senso-perception
12- Pseudo-psychiatric symptoms
13- Behavioral observations (impulsivity, perseveration ...
This article is merely informative, in Psychology-Online we do not have the power to make a diagnosis or recommend a treatment. We invite you to go to a psychologist to treat your particular case.
If you want to read more articles similar to Neuropsychology of Parkinson's Disease, we recommend that you enter our category of Neuropsychology.