http://www.psicologia-online.com/articulos/2009/01/modelo_etiologicos.shtml
Mental disorders are truly varied and can have their origin in a biological, dynamic, systemic or cognitive-behavioral cause. It is important to separate each of these possibilities well and to know their characteristics in order to establish an adequate diagnosis for the patient and offer the most appropriate treatment.
For this reason, in this PsicologíaOnline article, we are going to explain in detail the etiological models of mental disorders, including a practical case and its analysis.
Index
- Introduction to the etiological models of mental disorders
- CASE: 45-year-old male
- Analysis of the case study
- Predisposing factors
- Precipitating factors
- Maintaining factors
- Inhibitory factors
- Stability in goals
- The act of falling in love
- Etiopathogenesis of mental disorders
- Biologist model
- Drug treatment for OCD
- Cognitive-behavioral model
Introduction to the etiological models of mental disorders.
Nowadays there is a generalized thought about the etiology of abnormal behaviors as the unfolding of existing potentialities -to a certain extent- in all individuals, observing that the causes of the pathologies are manifested by virtue of a pluricausal convergence of terms biological, psychological and social determined. On the basis that when these elements were adequate in quality and quantity, then it would be possible the constitution of a healthy person, and in his absence or anomalous presence the origin of the psychopathology.
The specific action and / or reaction in each of the etiological factors inevitably has an impact on the others. It cannot be guaranteed that only one of them is the one that sets in motion the mechanism of pathological behaviors, or that It produces first an organic failure and then the psychopathological disorder, neither does the psychic trauma and its subsequent imprint biological. Everything is interrelated with any of these factors to end up being produced in an adverse situation, a mental discomfort and a biological circuit that allows and supports it. Variables of a quantitative or qualitative aspect are important, as well as their temporality, since they are determining conditions.
For example, short-term stimuli that are not repeated with sufficient periodicity tend to produce changes only at a quantitative and not qualitative level; only to acquire a certain quantitative value (different according to individual characteristics, even highlighting the idiosyncrasy of the time to interpret the subject), and now collaborating the persistence in time on the magnitude, it will have its translation in the aspect qualitative. Influencing long-term stimuli, having the ability to modify even genetic codes and affective stimuli.
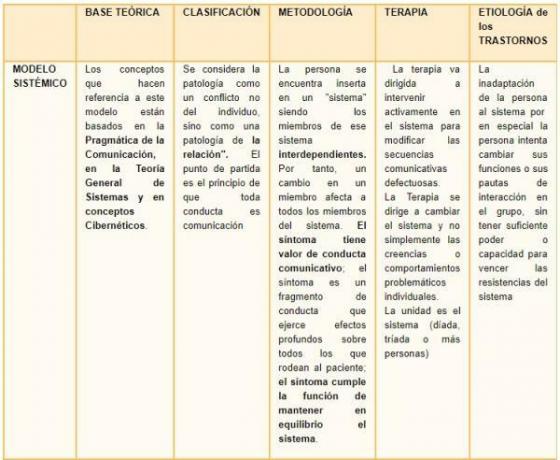
Theories and explanations help and complement each other to continue investigating the complexity of the human being, some through learning, others through of biology, of social relations... and all of them are nothing more than the parts of a whole to find the adaptive and healthy mechanisms for being human. As described below, the biologist models they look for the etiology in the physiology; psychoanalysis and dynamic models in the conformation of the self and the personality; the cognitive-behavioral models, in learning; and the systemic models in the relationship between the individual and other close systems. There are cases in which the biological predisposition indicated by an important hereditary load subtracts strength from the other variables, such as genetic abnormalities, but it seems demonstrated that the rest of the spectrum occurs in greater proportion in the disorders described by the Psychiatry.

CASE: 45-year-old male.
Only child of mature parents, (he was born when the mother was 43 years old and 40 years old father). Risk pregnancy, with losses and complete rest for nine months. The stage of his childhood was really dark and unhappy with a father diagnosed with schizophrenia and who, due to his delusions, kept this child and his wife in absolute silence because he believed that the noises in his head were caused by the two of them. Thus, the boy spent more hours in the street than at home and when he slept he covered his breathing with the bedding, so as not to provoke the ire of his father. In the marital relationship he was known infidelities, of which his young son was also a participant. His mother had to go to work because he had left his job as a representative of a well-known film production company, because they were persecuting him.
The patient's social relationships were limited to some friends from school and the neighborhood whom he did not take home so as not to create problems. But whose activities were always on the verge of illegality or the endangerment of physical integrity, with several car accidents to his credit.
At present the circle of friends is changing - in order not to discover his "oddities", he maintains two childhood friends, one of whom is already losing contact with him due to his supposed adherence to my friendship.
When he was a teenager and after warning from his father to his son, he hanged himself at home; being the first to find it. From here, their compulsive acts that they went to more and that today they persist to the point that his rituals occupy him more than 6 hours a day. He started knocking on the doors three times before leaving the house or before entering.
He has delusions like his father appears to them in their dreams sitting on the bed and a great need to do things very quickly. He also hears noises that cause him pain.
His relationship with his partner has not exceeded 2 years of permanence until his first marriage that lasted 14 years.
His job stability was intense, he had created a company in a cooperative system and later created several companies of finance and real estate in which he continues, his goal was to become the owner of a building in Madrid and not deprive himself of any whim.
His wife asked him to visit a specialist when he was 34 years old and his rituals and his impulsiveness for cleanliness, order and the control of all the members of his family and the members of his company was already a desperation, besides having been consuming cocaine for a long time - from the age of 29-, even a year before leaving home, he occasionally took this substance. He did not step on the white stripes of the zebra crossings, before crossing a traffic light he added all the license plates of the cars that were stopped and if they did not add an odd number he did not cross - To the point that one day the police called his home to come and pick him up because someone had seen him stopped at a traffic light on Genova street for more than an hour and a half without crossing; He would choose a word that he had said to himself or that he would have thought and he would repeat it an odd number that began at 3 and had no end, if he could not repeat them we would He made her repeat to us with tricks how to ask in different ways, he had a true obsession with having fun, he did not want to know anything about diseases, the medicine cabinet was full of state-of-the-art medications just in case, he sprayed all his clothes with bactericides, compulsively shopped, had excessive Concern for physical appearance - even that of family members, he was in charge of buying the clothes of all this - needed flattery permanently; this was one of his soothing, another the infidelities and feeling recognized.
He only felt relief when he achieved his envisioned purpose and then began another ritual. He never accepted his illness, they were just extravagant manias and if he was upset he would show quite a bit of hostility and mistrust.
He did not get the Business degree for lack of the English subject to which he never applied. His work is related to the world of finance and investment and is a extremely high stress level.
A 7-year-old son was born from their marriage relationship and after the initial joy caused him a lot of anxiety and fear. Subjected to treatment for the imposition of his wife, he breaks the relationship because he starts a new one.
Today he is 43 years old, he gave up psychotherapy and never took medicine.
Analysis of the practical case.
First note that it is a anxiety disorder and, therefore, reading related to these types of disorders will always be useful for the correct understanding of OCD. The DSM-IV criteria for the diagnosis of obsessive-compulsive disorder (APA, 1994): · 300.3 Obsessive-compulsive disorder.
TO. Obsessions or compulsions: The multiples already described
Obsessions are defined by:
(1) Recurring and persistent thoughts, impulses, or images that are experienced, sometime during the disturbance, as intrusive and inappropriate, causing marked anxiety or discomfort. In recent years, he had become tired and anxious that he could not stop them.
(2) The thoughts, impulses or images are not simply excessive worries about problems in everyday life. He was interested in death, in the appearances of faces on walls.
(3) The person tries to ignore or suppress such thoughts or impulses or neutralize them with some other thought or action. With compulsive actions.
(4) The person recognizes that the obsessive thoughts, impulses or images are a product of her own mind (not imposed as occurs in the insertion of thought). He knew that only or few people had these thoughts and that they were created by himself.
Compulsions are defined by:
(1) Repetitive behaviors (eg, hand washing, ordering, checking) or mental actions (eg, praying, counting, repeating words in silence) that the person feels compelled to perform in response to an obsession, or according to rules that must be rigidly applied. Those already mentioned.
(2) Mental behaviors or actions are aimed at neutralizing or reducing discomfort or some feared event or situation; however, these mental behaviors or actions are not realistically connected to what they are intended to neutralize or prevent, or are clearly excessive.
B. At some point during the course of the disorder, the person he acknowledges that obsessions or compulsions are excessive or irrational. Although he tried to hide them, when he detected them he could not stop talking about them and contrasting with the behaviors of others, always in a mocking tone as if it were an attitude nice.
C. Obsessions or compulsions produce marked discomfort; loss of time (in general, the individual spends more than an hour a day on them); or significantly interferes with routine habitual of the individual, with his professional activity, with his social activities or his relationships with others.
OCD implies a loss of control, on the part of the patient, of his thoughts and even his behavior. This fact, moreover, is experienced in a paradoxical way, as the patient recognizes such thoughts and / or behaviors as a product of himself. This leads to certain complications, such as the fact that the patient stops recognizing the excessiveness of his obsessions or compulsions, in short, that he has little awareness of the disease (an aspect that the DSM-IV explicitly calls the attention).
The etiology of OCD is multifactorial with an interaction, greater or less, of genetic, psychological and social factors Different theoretical frameworks coincide in proposing that it could be a combination of genetic, psychological and cultural aspects.
Predisposing factors.
They refer to individual characteristics, family and social situations that make the person more vulnerable to suffering from a disorder. They will increase the chances that a certain disorder will appear. These are the predisposing factors for mental disorders:
Inheritance
Some of the symptoms are already observed in his father, such as hostility, emotional instability, although he did not have self-destructive ideas, his aggressiveness diverted her towards others. Marital instability, aggressiveness is indicated in the father's text.
Personal variables
Risky, weird and weird behaviors Substance abuse: started when he was 29 years old Social skills: He was always shy and withdrawn and with few friends regarding his instability with his partners: It has been the general trend since he was 16 years old, and that continues to characterize his life adult ”.
Delusions
The fantasies that their father appears to them in their dreams sitting on the bed and the need to do things quickly
Personality
This unstable, aggressive way of behaving may have been learned and increased by drug use, but it is still completely may have a hereditary biological component, since her mother says that her paternal grandmother was treated by the family in a special way so that she would not suffer "shocks" and become moody.

Precipitating factors.
The factors that seem to influence the pathogenesis of the children of parents with psychiatric disorders would be the genetic factor, the age of the child, the quality of the parenting, the family environment, the occurrence of acute life events and chronic adversity, the number of sick parents and chronicity of the disease parental. Regarding the age of the child, the existing data support the idea that there are different conflicts and problems depending on the developmental period that the child is going through; It seems that the age between 0 and 5 years and the beginning of adolescence are the most vulnerable. As is the case in this case.
Parental inconsistency - parenting quality and family environment
All of these factors highlighted in bold have been precipitating factors, although chronic adversity is not can be attributed in maturity because their socio-affective and economic environment has been very favorable from the age of 25 years.
Family variable: As a child he has not received an education of trust and stability from his parents, but based on hypervigilance and fear, as well as economic adversity. Family split: there was no family split, until the death of the father, but it had an inconsistent and distrustful environment, the affectivity was mainly on the part of the mother, but having to work she could not overcome the feeling of abandonment. The family environment was therefore sordid and little enhancement of self-esteem and protection. In addition to being reduced to the parents and the maternal grandmother who sometimes lived with them sporadically.
The occurrence of acute life events and chronic adversity
In addition to the fear that he lived in his childhood with the behaviors of his father, the violent death of the same, leaving him a great feeling of guilt –Which occurred in the adolescence of the present case- and chronic economic adversity have been the most determining factors in the appearance of the TOC. The second acute crisis (since the death of his father) was precipitated by the birth of his son and by the imposition of his wife to see a specialist.
Maintaining factors.
The raw mourning, and the family economic situation of economic adversity, until he begins to work. The impossibility of maintaining permanent emotional relationships with other women whom he always mistrusts. Relationships with his closest friends always trying extreme situations, with a history of several car accidents, is that is, their aversion to risk (the compulsive) and risk seeking (the impulsive), as well as aggressive and unpredictable. Reducing more and more their social relationships.
Delusions
The fantasies that their father appears to them in their dreams sitting on the bed and the need to do things quickly Not wanting specialized help - avoidance -, permanent flight they are the most relevant maintenance factors in their behavior.
Inhibitory factors.
The main inhibiting factor is its compulsive acts, already mentioned above: the tension and anxiety that derive from obsessive thoughts, find relief through the performance of the compulsive act
Stability in goals.
Stability in the goals of keeping your job and being the owner and builder of a building in Madrid are more That fulfilled, until this moment the achievement of this allowed him to spend a few years without major crisis of the disorder that suffers. He sought refuge in his marriage and support in its stability without having acute crises until he had a child.
The act of falling in love.
The initial periods in his affective relationships are periods in which he feels accompanied, loved and reciprocated, all of which exert an inhibitory influence on the symptoms of the disorder.
Etiopathogenesis of mental disorders.
The existence of a multifactorial hypothesis in the etiology of OCD, but with a substrate predominantly biological in nature. Obsessive-compulsive disorder (OCD) is an etiologically heterogeneous and multidimensional pathology, even so, from the biological model it is studied from the following perspectives.
Today the treatments for OCD that have been shown to be effective in a controlled way are: exposure treatment with response prevention and psychopharmacological treatment. In addition, various varieties on them, include, mainly, cognitive treatment, modalities application (imaginary exposure, group treatment, family, etc.), and the treatments combined. So we proceed to describe the two models: biologist and cognitive-behavioral.
Biologist model.
These are the different hypothesis of the biological model:
- Serotonergic hypothesis: based on abnormal regulation of serotonin, since a serotonin reuptake inhibitor antidepressant reduces the intensity of symptoms in this type of disorder. Currently, a large number of serotonergic receptors have been identified and it is known that the most involved receptor is 5-HT1A, but it is not the only one.
- Dopaminergic hypothesis: Although serotonin is known to play a very important role in the disorder, the dopamine system is also affected, as evidenced by the existence of obsessive symptoms in Gilles de la Tourette syndrome and Parkinson's post-encephalitic. In both disorders, the basal ganglia are affected by dopaminergic dysfunction. Today it is believed that the dopaminergic system is involved in certain subtypes of atypical OCD: comorbid with tics and comorbid with psychotic symptoms.
- Autoimmune hypothesis: in autoimmune diseases that affect the basal ganglia, such as Sydenham's chorea, obsessive-compulsive symptoms appear together with motor phenomena and even earlier.
- Genetic hypothesis: Studies in relatives generally reveal a prevalence rate that ranges from 0 to 36%, which suggests the existence of genetic factors involved in OCD. In recent studies among homozygous twins, heterozygous twins and the Pauls studies, the evidence of family disorders implicated in this entity is consolidated. However, it seems clear that heredity cannot fully explain the expression of OCD, requiring additional factors to modify this previous genetic vulnerability.
Furthermore, advances in neuroimaging techniques have made it possible to observe hemodynamic alterations in the parts of the brain involved in OCD. Hyperfunction of the orbitofrontal cortex has been described with positron emission tomography in OCD, clearly differentiating it from depressive disorders and schizophrenia, where a hypofunction of the same area. The joint use of behavioral techniques and neuroimaging tests will allow a better understanding of the functions and location of the areas involved in this disorder. Recent studies show that the provocation of obsessive-compulsive symptoms is correlated with an increase in flow in the orbitofrontal cortex and with alterations of the caudate nucleus. It is interesting to note that the result of these techniques to assess the effects of treatment is independent, whether it is a behavioral or pharmacological treatment.
In conclusion: the serotonergic theory remains basic for the pathogenesis of OCD, but not sufficient, leaving the investigation on the implication of the basal ganglia and the dopaminergic system, without ruling out autoimmune or other factors (neuropeptides, arginine, vasopressin, oxytocin and somatostatin) that could help shed light on the various subtypes of OCD and its incardination within the spectrum disorders in the future obsessive compulsive.
Drug treatment for OCD.
Psychotropic drugs have been widely used in the OCD treatment. For a long period, from the 1960s to the 1990s, the drug used has been clomipramine (Anafranil), an antidepressant tricyclic to which its efficacy has traditionally been associated with the reduction of depressive symptoms (Marks et al., 1980).
At the end of the 1980s, a set of new drugs appeared, the selective serotonin reuptake inhibitors (SSRIs), which, supported by the role that serotonin seems to play in OCD (Barr, Goodman and Price, 1992), have represented an important step in the pharmacological treatment of this disorder. The efficacy of SSRIs does not appear to be linked to the existence of depressive symptoms, and also have fewer side effects than clomipramine (Rasmussen, Eisen and Pato, 1993, Freeman et al., 1994).

Cognitive-behavioral model.
Unlike the previous models, which place the causes on factors of internal development of the people, the cognitive-behavioral models explain psychopathology on the basis of learning inappropriate responses to environmental factors.
These models recognize that genetic and biological factors pose structural limitations on which learning operates. They also recognize that there are disorders that are not the result of learning, such as autism, psychotic disorders or bipolar disorder.
Its greatest contribution is that open the possibility of action to the individual (and the therapist) to try to overcome his limitations.
The psychodynamic treatments of the past achieved transitory improvements, which is why OCD acquired a reputed reputation as an intractable problem (Coryell, 1981). Later, from the Behavior Therapy, the initial approaches were also problematic. Indeed, although there was an improvement in the treatment of the problem, it was limited. The application of thought arrest and other procedures based on contingency control were only useful in a small percentage of patients (less than 50%) (Stern, 1978). The situation improved with the application of the techniques used in other anxiety disorders, more specifically with phobias. The application of systematic desensitization and other techniques such as paradoxical intention focused on verbalization repetition of obsessive thoughts, facilitated the approach to OCD although not significantly (Beech and Vaughan, 1978). OCD resisted the potency demonstrated by Behavioral Therapy treatment for anxiety disorders.
However, a specific method of cognitive behavioral therapy call "prevention of exposure and reaction"It is effective for many people with OCD. This method implies that the patient faces, deliberately or voluntarily, the feared object or idea, either directly or with the imagination. At the same time, the patient is encouraged to abstain from his rituals with support and structure provided by the therapist, and possibly others that the patient recruits to assist him. For example, a person who washes his / her hands compulsively may be encouraged to touch an object that he / she believes is contaminated and then the person is urged to avoid washing for several hours until the anxiety provoked has been reduced by much. Treatment then proceeds step by step, guided by the patient's ability to tolerate anxiety and control rituals. As treatment progresses, most patients gradually feel less anxiety caused by obsessive thoughts and are able to resist compulsive urges.
The behavioral ERP therapy emphasizes changing the beliefs and thinking patterns of the patient with OCD; Starting from one of Albert Ellis's theories from which psychopathological problems are explained by the system of Inappropriate beliefs (irrational beliefs) to face their daily life and therefore offering answers inadequate.
The cognitive contribution qualifies both the factors related to acquisition and maintenance. In the genesis of the disorder, the initial consideration of the problem as normal and the passage to the pathological depending on the assessment and its interpretation, supposes an advance on the conditioning model and a better explanation of how the disorder. This means, from the therapeutic point of view, influencing how the patient evaluates and interprets intrusive thoughts. On the other hand, and with regard to the maintenance of the problem, emphasis is placed on responsibility, on the awareness of the patient to reduce the existing danger.
From the cognitive-behavioral approach, the modification of cognitive behavior is emphasized through the cognition (products, processes, interpretation ...) and cognitive structures (beliefs, values).
The meta-analysis of van Balkom et al. (1994) conclude that ERP, alone or in combination with SSRIs, is more effective than SSRI drugs alone.




This article is merely informative, in Psychology-Online we do not have the power to make a diagnosis or recommend a treatment. We invite you to go to a psychologist to treat your particular case.
If you want to read more articles similar to Etiological models of mental disorders, we recommend that you enter our category of Clinical psychology.
Bibliography
- http://www.psicothema.com/psicothema.asp? id = 464
Steketee, G.S. Frost, R.O. (1998). Obsessive-compulsive disorder. In A.S. Bellack and M. Hersen (eds.), Comprehensive Clinical Psychology. Vol. 6 (pp. 367-398). Amsterdam: Pergamon - http://www.psicologia-online.com/ESMUbeda/Libros/Manual/manual22.htm